8 Ways to Improve Your Medical Claims Billing Process
Medical Billing / RCM | Practice Management
The medical billing process is a series of steps completed by billing specialists to ensure that medical professionals are reimbursed for their services. Depending upon the circumstances, it can take a matter of days to complete, or may stretch over several weeks or months. While the process may differ slightly between medical offices, here is a general outline of a medical billing workflow.
Patient Registration
Patient registration is the first step on any medical billing flow chart. This is the collection of basic demographic information on a patient, including name, birth date, and the reason for a visit. Insurance information is collected, including the name of the insurance provider and the patient's policy number, and verified by medical billers. This information is used to set up a patient file that will be referred to during the medical billing process.
Financial Responsibility
The second step in the process is to determine financial responsibility for the visit. This means looking over the patient's insurance details to find out which procedures and services to be rendered during the visit are covered. If there are procedures or services that will not be covered, the patient is made aware that they will be financially responsible for those costs.
Superbill Creation
During check-in, the patient will be asked to complete forms for their file, or if it is a return visit, confirm or update information already on file. Identification will be requested, as well as a valid insurance card, and co-payments will be collected. Once the patient checks out, medical reports from the visit are translated into diagnosis and procedure codes by a medical coder. Then, a report called a “superbill” may be compiled from all the information gathered thus far. It will include provider and clinician information, the patient's demographic information and medical history, information on the procedures and services performed, and the applicable diagnosis and procedure codes.
Claims Generation
The medical biller will then use the superbill to prepare a medical claim to be submitted to the patient's insurance company. Once the claim is created, the biller must go over it carefully to confirm that it meets payer and HIPPA compliance standards, including standards for medical coding and format.
Claims Submission
Once the claim has been checked for accuracy and compliance, submission is the next step. In most cases, the claim will be electronically transmitted to a clearinghouse, which is a third-party company that acts as a liaison between healthcare providers and health insurers. The exception to this rule are high-volume payers, such as Medicaid, who will accept claims directly from healthcare providers.
Monitor Claim Adjudication
Adjudication is the process by which payers evaluate medical claims and determine whether they are valid and compliant, and if so, the amount of reimbursement the provider will receive. During this process, the claim may be accepted, rejected or denied. An accepted claim will be paid according to the insurers agreements with the provider. A rejected claim is one that has errors that must be corrected and the claim resubmitted. A denied claim is one that the payer refuses to reimburse.
Patient Statement Preparation
Once the claim has been processed, the patient is billed for any outstanding charges. The statement generally includes a detailed list of the procedures and services provided, their costs, the amount paid by insurance and the amount due from the patient.
Statement Follow-Up
The last step in the medical billing process is to make sure bills are paid. Medical billers must follow up with patients whose bills are delinquent, and, when necessary, send accounts to collection agencies.
Today’s healthcare system is evolving rapidly, not just with regard to patient needs and new treatment developments, but also in the often unseen arena of medical coding and billing. While much of healthcare is front and center between the doctor and patient, much is still left to be done when the patient leaves the doctor’s office or hospital. For those who manage this behind the scenes, it can often become overwhelming with the ever-constant changes in guidelines and regulations. The medical billing process, however, is vital to healthcare providers as it allows them to receive reimbursement for the treatment provided to patients, and thus keep their doors open for business. What are the basics when it comes to medical billing and what avenues are available to help?
1. What is Medical Billing?

Unlike
most everyday transactions where you receive a service or product and
promptly pay the bill, medical billing is a much more complex
transaction.
On every patient’s chart, the healthcare provider
documents what services or procedures were performed and provides a
diagnosis. That text is then translated into codes by a medical coder,
each code indicating what was done or used by the physician and why.
Next, a medical biller uses those codes, now called a superbill, to
comprise a claim that will be sent to the patient’s insurance company.
When the claim is approved, the healthcare provider will receive
reimbursement for the services provided. The provider's billing
department will then attempt to recover the out of pocket expense from
the patient. This is often done by sending invoices in the mail and
manually calling the patient to remind them to pay their bill.
Recovering patient out of pocket costs is increasingly becoming more
important to providers as out of pocket costs have risen 37% since 2009.
2. The Process of Medical Billing

The very first step involves registering the patient, and obtaining their personal and insurance information. Based on a patient’s insurance plan, a medical biller can determine what services will be covered and which ones the patient will be responsible for, including co-payments. After the patient has checked out, a medical coder applies codes for the diagnosis and procedures performed, creating a superbill. From here the medical biller creates a claim including the cost of each procedure. The medical biller must be careful to ensure that the claim is “clean” or is in compliance with state and federal regulations for coding and format. Some healthcare practices decide to even use a third party, known as a clearinghouse, to format claims according to the specifications of each insurance company and in accordance with HIPAA. It’s clear to see that one must be educated on the ins and outs of this process or it could easily result in a denied or rejected claim, which means no reimbursement.
3. How to Become a Medical Billing Specialist

In
many practices and offices, employees may have to wear many hats,
medical biller being one of them. It’s no secret that this role is a
serious one, with the financial health of a practice relying on the
competent performance of the medical billers. Medical billers must have a
grasp of medical codes and current regulations, and they must also be
good communicators with healthcare professionals and with patients when
collections must be made. There are many training programs
available to help prepare one for the CPB (Certified Professional
Biller) course. Most training programs offer invaluable and up-to-date
information pertaining to health insurance and different reimbursement
methods, to ensure claims are accepted.
Communication with the
payer (insurance company) and individual patients may be a long process.
Therefore, it’s important for the medical biller to maintain healthy
relationships with the patients. The goal of the medical biller to is
make sure bills get paid, but not at the sacrifice of patient loyalty. Enter provides software
to suit the needs of you and your patients from the start. Enter helps
you to easily keep track of your customers, their balances, and payment
history. With advanced machine learning, Enter’s AI can determine which
communication format your customers prefer based on their demographics,
knowing when to text, email, call, or send a letter on your behalf. With
mobile banking and interest-free payment plans, collections can be made
conveniently and regularly. Enter can help to simplify a complex
situation. To see how you could get started for free checkout our pricing page.
4. Physician and Hospital billing-What’s the difference?
Physician billing, also known as professional billing is the billing of claims for work that was performed by a physician or other healthcare professionals, including inpatient and outpatient services. Most all of these claims are billed electronically as the 837-P form. The paper equivalent of this form is CMS-1500. Institutional or hospital billing deals with claims for work or procedures performed by institutions such as hospitals, nursing facilities, as well as inpatient and outpatient centers. These claims require the UB-04 paper form or the 837-I electronic version. Hospital, or institutional, billing is usually more complex and requires dedicated billers along with dedicated coders. When it comes to physician billing, many times these roles are combined.
5. Major or Necessary Forms
Superbill or Encounter form

The first major form to be generated for medical billing is a superbill, also known as an encounter form. This form is created by the medical coder after a patient has seen the doctor. The medical coder uses the information from the patient’s chart to note what diagnosis was made, what procedures were performed, what services or prescriptions were given, etc. This information is then processed into codes. The main types of codes you will see on a superbill are ICD codes (International Classes of Diseases) used for diagnosis, CPT codes (Current Procedure Terminology) for medical procedures, and HCPCS codes (Healthcare Common Procedure Coding System) for procedures or equipment not covered under CPT codes. Many practices have a preset list of common codes used by their physicians to speed up the coding process. The superbill is essential for reimbursement and must be accurately filled in before being submitted as a claim. The superbill must list the provider along with location of treatment and a signature with an NPI number. Patient information must be complete, including demographics and insurance information.
Explanation of Benefits

This is a form sent to providers and patients from the insurance company after their claim has been evaluated. It may look like a bill to the patient, but it is actually sent to inform them of what was included in the healthcare claim submitted by their physician. It includes the services provided, the physician fees, what part of the fee the insurance company will cover, and what the patient is responsible for covering. The EOB forms are not only used by insurance companies to inform their beneficiaries of what charges were made, but they also have a role in identifying healthcare fraud stemming from unnecessary charges.
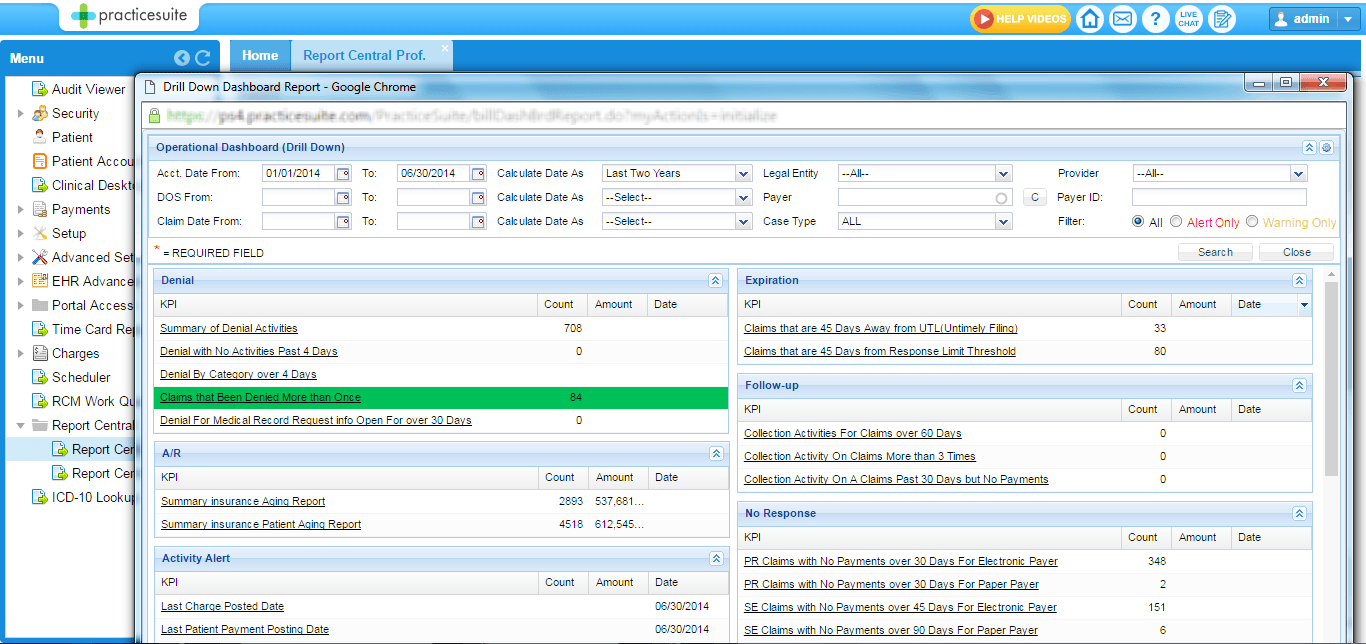
6. Revenue Cycle Management

Revenue Cycle Management or RCM is a broad term encompassing the initial patient appointment to coding and billing, to sending in a claim, and finally to reimbursement for healthcare services provided. Many offices and healthcare institutions implement electronic software to expedite and ensure a smooth claims process. By using electronic software, healthcare professionals are able to track the status of claims sent, and address any denied claims or delays in reimbursement. By having a good internal RCM set up, healthcare providers are able to quickly resolve issues and ensure a steady revenue.
7. Medical Billing Software
It
would be hard to find an office or institution that didn’t use some
form of medical billing software. The use of even basic software allows
for electronic entry of patient demographics, insurance information,
procedures and coding with just a few clicks. Superbills are generated
through such software and even sent as claims to Medicare and other
insurance companies. More sophisticated forms of billing software are
able to recall all diagnosis and procedure codes available, and can even
be linked to other independent software to meet a particular billing
need. Such software is able to recall patient and provider information
based on previous claims, allowing the user to update the bill by adding
or deleting items to the claim. While medical billing software is a
necessity, there is room for caution.
According to HBMA
(Healthcare Billing & Management Association) more than 70% of
consumers have been scammed by a misleading ad or internet opportunity
for medical claims processing. Before investing in any software, do your
research and reach out to reputable sources. In short, automation helps
with managing data and helps ensure that claims for reimbursement will
meet the different standards for claim acceptance.
8. EMR vs EHR vs PHR

Put simply Electronic medical records (EMRs) are a digital version of a paper chart. The patient’s medical and treatment history included in the EMR is limited to the one facility it was generated in. An EMR is good for tracking data over time and improving overall care of the patient, but it is limited to that one facility. If, for example, a patient were to switch doctors or require any of their past records, it would possibly need to be printed or put on a disc. The EMR works well within the walls of a practice, but it doesn’t travel well. An Electronic health record (EHR) on the other hand, not only has clinical patient data from the doctor’s office, but includes data from other health care providers, laboratories, and even specialists that have treated the patient. Basically, it’s a record of all the healthcare a patient has received. EHRs travel where the patient does, meaning that other healthcare professionals involved with that patient’s care can access their records. Personal health records (PHRs) are health records designed to be managed by the patient. They are separate and do not replace the legal record of healthcare providers. PHRs serve to help patients manage their own health information.
Here are some great companies that Enter works with
who specialize in EMR, EHR and PHR. Enter, by directly integrating with a
vast array of EMRs, EHRs, and PHRs, can provide auto adjudication,
estimation and instant collection services for providers.
Enter has the unique ability to directly integrate with EMRs, EHRs and PHRs like AdvancedMD, AllMeds, Allscripts, athenahealth, Cerner, CPSI, drchrono, eClinicalWorks, Emdeon, Epic, Exscribe, Flatiron, GE Centricity, Greenway, IKnowMed, MAeHC, McKesson, Meditech, MediTouch/HealthFusion, Mosaiq, MTBC, NextGen, Orchard LIS, Ortho Phoenix, Raintree, QRS, SRS, Star, countless homegrown EHRs, a handful of HIEs, and installing with more every day.
9. Contractual Adjustment
A more common term used for this is a write-off, meaning it’s not paid. This adjustment in a patient’s bill is between the insurance plan and the provider. This contractual arrangement is made when the provider agrees to accept an insurance plan. The insurance plan agrees to pay a set amount for various services. If a provider charges more than what the insurance plan will pay, this is where the write-off occurs. While providers may not receive what they originally charged, they are guaranteed to receive a significant portion. Write-offs are only made on services covered by the insurance company.
10. Insurance Claim Process

After
the superbill has been completed and reviewed by the medical biller, it
is either put into a paper claim form or an electronic form. It may
then be sent to a clearinghouse for further evaluation and to ensure it
is formatted according to HIPAA and specific insurance guidelines.
From
there the claim is finally submitted to the insurance company where it
will be evaluated. Now that the claim is in the payer’s hands, they
evaluate the medical claim and decide whether the claim is valid and how
much they will reimburse the provider for. It is also at this point
that the claim may be denied or rejected. If there are any errors, the
provider can enter into an appeal process with the insurance company.
11. Patient Payment Process

Once the payer has reviewed the claim, accepted it, and paid the agreed upon portion of services rendered, the provider now is ready to bill the patient. Typically, whatever portion the insurance didn’t cover, the patient is responsible for. Medical billers are in charge of sending out the medical bills and following up with patients who have not paid. Each provider and facility has different guidelines regarding bill payments and contacting patients who are delinquent in their payments. A worst-case scenario may involve enlisting the help of a collection agency. This is another fee the provider will have to pay for. Enter may be a better solution. From the start of a patient’s care, Enter determines what kind of communication the patient prefers based on machine learning and our AI’s recommendation. When billing time arrives, patients are able to receive text messages, emails, phone calls, or even letters to notify them of pending payments. This avoids the need for collection agencies and allows the patient to pay with ease and based on their budget. Mobile banking and interest-free payment plans keep patients out of collections and enable providers to effectively recover past-due revenue.
12. Managed Care Provider/Third party Payer System

There
are many types of insurance plans available to the public today.
Managed care organizations (MCOs) are the most prevalent and widely used
compared to indemnity plans. While indemnity plans allow you to see
whichever provider you desire, they are much more expensive than MCOs.
MCOs aim to reduce healthcare costs by providing a selected network of
providers and facilities and restricting where a patient can receive
treatment. There are three main types we will overview.
The first
is Health Management Organizations (HMOs). The premium for HMOs is
lower, but allows for almost no flexibility when it comes to choosing
providers outside of network. Medical care is prearranged with a list of
medical services that will be provided. When it comes to seeing a
specialist, the primary care provider decides if it is necessary and
must first provide a referral.
A Preferred Provider Organization
(PPO) has higher premiums but allows patients to see providers outside
of network if they choose to. However, sticking with a preferred
provider in network gives patients a cheaper option.
Point of
Service (POS) is a cross between the HMO and PPO. Under this plan
patients are encouraged to stay within the network by lower fees, but
they also have the option of to go out-of-network for a higher fee.
Consumer-Driven
Health Plan (CDHP) has low premiums with a high deductible. When the
deductible is met, subscribers receive benefits much like a PPO.
13. AAPC Certifications
The Certified Outpatient Coder (COC) certificate, formerly known as CPC-H, is highly recommended for coders and medical billers. This certificate verifies that a medical biller/coder is specialized in outpatient billing and coding, and educated in the unique challenges faced in medical billing, including: coding rules, regulations, claim denials, and correct claim form completion. Check out the AAPC website for more information about the COC exam.
Comments
Post a Comment